- Amman, King Hussain Park, Jordan
- +(962) 000-0000
- info@curafile.com
Chronic Obstructive Pulmonary Disease (COPD)
- Home
- Lungs and Breathing
- Chronic Obstructive Pulmonary Disease (COPD)
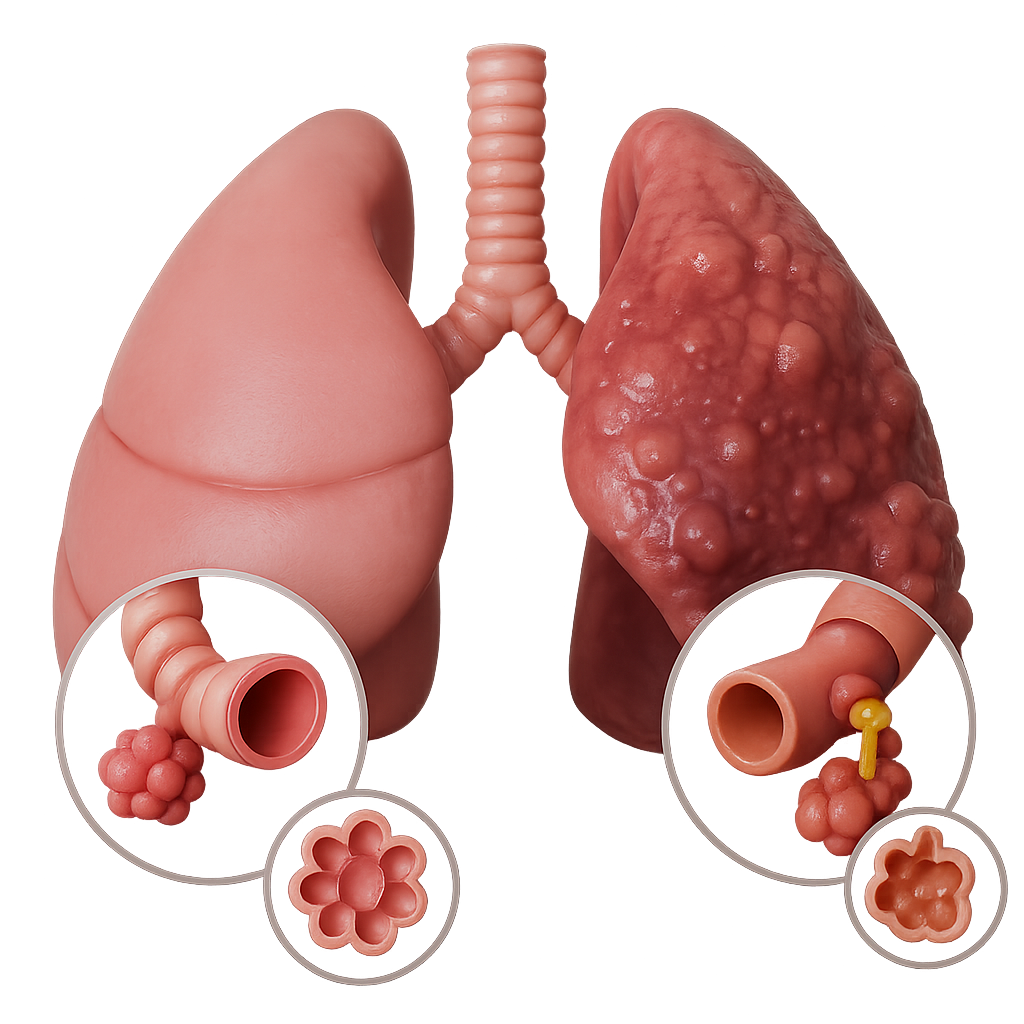
Chronic obstructive pulmonary disease (COPD) is a common lung disease. Having COPD makes it hard to breathe.
There are two main forms of COPD:
- Chronic bronchitis, which involves a long-term cough with mucus
- Emphysema, which involves damage to the lungs over time
Most people with COPD have a combination of both conditions.
COPD symptoms often don’t appear until a lot of lung damage has occurred. Symptoms usually worsen over time, especially if smoking or other irritating exposure continues.
Symptoms of COPD may include:
- Trouble catching your breath, especially during physical activities.
- Wheezing or whistling sounds when breathing.
- Ongoing cough that may bring up a lot of mucus. The mucus may be clear, white, yellow or greenish.
- Chest tightness or heaviness.
- Lack of energy or feeling very tired.
- Frequent lung infections.
- Losing weight without meaning to. This may happen as the condition worsens.
- Swelling in ankles, feet or legs.
People with COPD also are likely to have times when their symptoms become worse than the usual day-to-day variation. This time of worsening symptoms is called an exacerbation (eg-zas-er-bay-shun). Exacerbations can last for several days to weeks. They can be caused by triggers such as smells, cold air, air pollution, colds or infections. Symptoms may include:
- Working harder than usual to breathe or having trouble breathing.
- Chest tightness.
- Coughing more often.
- More mucus or changes in mucus color or thickness.
- Fever.
You get fluoride from toothpaste, water, and other sources. This fluoride, along with your salvia, helps the enamel repair itself by replacing the minerals. Your teeth go through this natural process of losing minerals and regaining minerals all day long. But if you don’t take care of your teeth and/or you eat and drink lots of sugary or starchy things, your enamel will keep losing minerals. This leads to tooth decay.
A white spot may appear where minerals have been lost. This is an early sign of tooth decay. You may be able to stop or reverse the decay at this point. Your enamel can still repair itself, if you take better care of your teeth and limit sugary/starchy foods and drinks.
But if the tooth decay process continues, more minerals are lost. Over time, the enamel is weakened and destroyed, forming a cavity. A cavity is a hole in your tooth. It is permanent damage that a dentist has to repair with a filling.
The main cause of COPD in developed countries is tobacco smoking. In the developing world, COPD often occurs in people exposed to fumes from burning fuel for cooking and heating in homes that don’t have good airflow. Long-term exposure to chemical fumes, vapors and dusts in the workplace is another cause of COPD.
Not all people who have smoked for a long time have COPD symptoms, but they may still have lung damage, so their lungs don’t work as well as they used to. Some people who smoke get less common lung conditions that may be diagnosed as COPD until a more thorough exam shows a different diagnosis.
Often COPD can be hard to diagnose because symptoms can be the same as those of other lung conditions. Many people who have COPD may not be diagnosed until the disease is advanced.
To diagnose your condition, your healthcare professional reviews your symptoms and asks about your family and medical history and any exposure you’ve had to lung irritants — especially cigarette smoke. Your healthcare professional does a physical exam that includes listening to your lungs. You also may have some of these tests to diagnose your condition: pulmonary function tests, lab tests and imaging.
Pulmonary function tests
Pulmonary function tests are done to find out how well your lungs are working. These tests may include:
- Spirometry. In this test, you breathe out quickly and forcefully through a tube connected to a machine. The machine measures how much air the lungs can hold and how quickly air moves in and out of the lungs. Spirometry diagnoses COPD and tells how much airflow is limited.
- Lung volume test. This test measures the amount of air the lungs hold at different times when breathing in and out.
- Lung diffusion test. This test shows how well the body moves oxygen and carbon dioxide between the lungs and the blood.
- Pulse oximetry. This simple test uses a small device placed on one of your fingers to measure how much oxygen is in your blood. The percentage of oxygen in the blood is called oxygen saturation. You also may have a six-minute walking test with a check of your oxygen saturation.
- Exercise stress test. An exercise test on a treadmill or stationary bike may be used to monitor heart and lung function during activity.
Imaging
- Chest X-ray. A chest X-ray may show some lung changes from COPD. An X-ray also can rule out other lung problems or heart failure.
- CT scan. A CT scan combines X-ray images taken from different angles to create images of structures inside the body. A CT scan gives much greater detail of changes in your lungs than a chest X-ray does. A CT scan of your lungs can show emphysema and chronic bronchitis. A CT scan also can help tell if you might benefit from surgery for COPD. CT scans can be used to check for lung cancer.
Pulmonary function and imaging tests also can be used to check your condition over time and see how treatments are working.
Lab tests
- Arterial blood gas analysis. This blood test measures how well your lungs are bringing oxygen into your blood and removing carbon dioxide.
- Testing for AAT deficiency. Blood tests can tell if you have the genetic condition called alpha-1-antitrypsin deficiency.
- Blood tests. Blood tests aren’t used to diagnose COPD, but they may be used to find the cause of your symptoms or rule out other conditions.
Treatment is based on how severe your symptoms are and whether you often have bouts when symptoms get worse. These bouts are called exacerbations. Effective therapy can control symptoms, slow how fast the condition worsens, lower the risk of complications and improve your ability to lead an active life.
The most essential step in any treatment plan for COPD is to quit all smoking. Stopping smoking can keep COPD from getting worse and making it harder to breathe. But quitting smoking isn’t easy, especially if you’ve tried to quit and haven’t been successful.
Talk with your healthcare professional about stop-smoking programs, nicotine replacement products and medicines that might help. Also talk about how to handle relapses. Your healthcare professional may recommend a support group for people who want to quit smoking. Also, stay away from secondhand smoke whenever possible.
Several kinds of medicines are used to treat the symptoms and complications of COPD. You may take some medicines on a regular basis and others as needed.
Most medicines for COPD are given using an inhaler. This small hand-held device delivers the medicine straight to your lungs when you breathe in the fine mist or powder. Talk with your healthcare professional so that you know the right way to use the inhaler prescribed.
Medicine also can be given using a nebulizer. This small machine has a mask or mouthpiece and a hose attached to a round cup for liquid medicine. The nebulizer changes liquid medicine into a mist so it can be breathed into the lungs. Nebulizers also help loosen mucus. You may have one of these types of nebulizers:
- Compressor or jet nebulizers force air through the medicine to create mist.
- Ultrasonic nebulizers use high-frequency vibrations to create mist.
- Mesh or membrane nebulizers push the medicine through a mesh cap with tiny holes to create mist.
Bronchodilators
Bronchodilators are medicines that usually come in inhalers. Bronchodilators relax the muscles around the airways. This can help relieve coughing and make breathing easier. Depending on how severe your COPD is, you may need a short-acting bronchodilator before activities, a long-acting bronchodilator that you use every day or both.
Examples of short-acting bronchodilators include:
- Albuterol (ProAir, Ventolin, Proventil).
- Ipratropium (Atrovent).
- Levalbuterol (Xopenex).
An example of a short-acting bronchodilator combination inhaler is ipratropium bromide-albuterol (Combivent Respimat).
Inhaled steroids
Inhaled corticosteroids, often simply called steroids, can lessen airway inflammation and help prevent bouts when COPD symptoms get worse. Side effects of inhaled steroids may include bruising, mouth infections and hoarseness. These medicines are useful if you often have times when COPD symptoms get worse.
Combination inhalers
Some combination inhalers include more than one type of bronchodilator. Examples of these include:
- Aclidinium bromide-formoterol fumarate (Duaklir Pressair).
- Glycopyrrolate-formoterol fumarate (Bevespi Aerosphere).
- Tiotropium bromide-olodaterol (Stiolto Respimat).
- Umeclidinium-vilanterol (Anoro Ellipta).
Other inhalers combine bronchodilators and inhaled steroids. Examples include:
- Budesonide-glycopyrrolate-formoterol fumarate (Breztri Aerosphere).
- Fluticasone-vilanterol (Breo Ellipta).
- Fluticasone furoate-umeclidinium-vilanterol (Trelegy Ellipta).
- Budesonide-formoterol (Breyna, Symbicort).
- Fluticasone propionate-salmeterol (Advair, AirDuo RespiClick, Wixela Inhub).
Oral steroids
For times when COPD symptoms get worse, short courses of oral corticosteroids — for example, 3 to 5 days — may prevent more worsening of COPD. Oral corticosteroids are medicines taken by mouth. Long-term use of these oral medicines can have serious side effects, such as weight gain, diabetes, osteoporosis, cataracts and higher risk of infection.
Phosphodiesterase-4 inhibitors
A medicine approved for severe COPD and symptoms of chronic bronchitis is roflumilast (Daliresp), a phosphodiesterase-4 inhibitor. This medicine lessens airway inflammation and relaxes the airways. Common side effects include nausea, diarrhea and weight loss. Roflumilast is used to prevent exacerbations and lessen how often they happen.
Theophylline
When other treatment has not been effective or if cost is a factor, theophylline (Elixophyllin, Theo-24, Theochron), a less expensive medicine, may help make breathing easier and prevent bouts when symptoms get worse. Side effects depend on the dose and may include nausea and trouble sleeping. Blood tests are commonly used to monitor blood levels of theophylline. Irregular heartbeats and seizures are possible if the blood level is too high.
Antibiotics
Respiratory infections, such as acute bronchitis, pneumonia and influenza, can make COPD symptoms worse. Antibiotics may help treat these bouts of worsening COPD symptoms, but they aren’t generally recommended to prevent infections. Some studies show that certain antibiotics, such as azithromycin (Zithromax), help prevent COPD exacerbations. But side effects and antibiotic resistance may limit their use.
Oxygen therapy, a pulmonary rehabilitation program and in-home noninvasive ventilation therapy can all help treat COPD.
Oxygen therapy
If there isn’t enough oxygen in your blood, you may need supplemental oxygen. You can get this extra oxygen to your lungs through a mask or through plastic tubing with tips that fit into your nose. These attach to an oxygen tank. Lightweight, portable units that you can take with you can help you be more mobile.
Some people with COPD use oxygen only during activities or while sleeping. Others use oxygen all the time. Oxygen therapy can improve quality of life and extend life. Talk with your healthcare professional about your needs and oxygen therapy options.
Pulmonary rehabilitation program
These programs usually combine health education, exercise training, breathing techniques, nutrition advice and counseling. You work with a variety of specialists who can tailor your rehabilitation program to meet your needs.
Pulmonary rehabilitation after bouts of worsening symptoms may lessen the likelihood that you’ll need to go back into the hospital. Pulmonary rehabilitation also allows you to participate more fully in everyday activities and improves your quality of life. Talk with your healthcare professional about attending a program.
This therapy may prevent bouts of worsening symptoms for some people with severe COPD. Research is ongoing to determine the best ways to use this therapy at home.
Evidence supports in-hospital use of breathing devices, such as bilevel positive airway pressure (BiPAP). BiPAP may help certain people with COPD if used at home during the night. A noninvasive ventilation therapy machine attaches to a mask worn over your mouth and nose. BiPAP helps to make breathing easier and may lessen the likelihood of going back into the hospital. It also lowers how much carbon dioxide is left behind in your lungs when you breathe out. Too much carbon dioxide may lead to acute respiratory failure and the need to be in the hospital.
Even with ongoing treatment, you may have times when symptoms become worse for days or weeks. These are called exacerbations, and they may lead to lung failure if you don’t receive treatment right away.
Exacerbations may be caused by a respiratory infection, air pollution or other triggers that worsen irritation and inflammation in the lungs. Whatever the cause, it’s important to get medical help right away if you notice a cough that seems worse than usual or a change in the mucus you cough up, or you have a harder time breathing.
When exacerbations happen, you may need medicines such as antibiotics, steroids or both; supplemental oxygen; or treatment in the hospital. Once symptoms get better, your healthcare professional can talk with you about ways to prevent bouts of worsening symptoms in the future. You may need to quit smoking; take inhaled steroids, long-acting bronchodilators or other medicines; get your annual flu vaccine; and avoid air pollution whenever possible.
Surgery is an option for some people with some forms of severe emphysema that aren’t helped enough by medicines alone. Surgical options include:
- Lung volume reduction surgery. In this surgery, the surgeon removes small wedges of damaged lung tissue from the upper lungs. This creates extra space in the chest so the healthier lung tissue that remains can expand and the muscle that helps in breathing, called the diaphragm, can work better. In some people, this surgery can improve quality of life and help them live longer.
- Endoscopic lung volume reduction. Also called endobronchial valve surgery, this is a minimally invasive procedure to treat people with COPD. A tiny one-way endobronchial valve is placed in the lung. Air can leave the damaged part of the lung through the valve, but no new air gets in. This allows the most damaged lobe to shrink so that the healthier part of the lung has more space to expand and function.
- Lung transplant. A lung transplant may be an option for certain people who meet specific criteria. Replacing a lung can make breathing easier and allow a more active lifestyle. But it’s major surgery that has significant risks, such as organ rejection. A lung transplant requires taking lifelong medicine that weakens the immune system.
- Bullectomy. Large air spaces called bullae form in the lungs when the inner walls of the alveoli are destroyed. This leaves one large air sac instead of a cluster of many smaller ones. These bullae can become very large and cause breathing problems because old air is trapped and there isn’t room for new air to get in. In a bullectomy, the surgeon removes the bullae from the lungs to help improve air flow.
If you have COPD, you can take steps to feel better and slow the damage to your lungs:
- Control your breathing. Talk with your healthcare professional or respiratory therapist about methods for breathing more efficiently throughout the day. Also talk about positions that make breathing easier; ways to conserve your energy, such as sitting for tasks when possible; and ways to relax when you have trouble catching your breath.
- Clear your airways. With COPD, mucus tends to collect in air passages and can be hard to clear. Removing mucus with controlled coughing, drinking plenty of water and using a humidifier may help.
- Get regular physical activity. It may seem difficult to be active when you have trouble breathing. But regular physical activity and exercise can improve your overall strength and endurance and strengthen the muscles you use to breathe. Talk with your healthcare professional about which activities are best for you.
- Eat healthy foods. Eating healthy foods can help you keep your strength. If you’re underweight, your healthcare professional may recommend nutritional supplements. If you’re overweight, losing weight can greatly help your breathing, especially during physical activities.
- Avoid smoke and poor-quality air. In addition to quitting smoking, it’s important to avoid places where others smoke. Secondhand smoke may add to lung damage. Air pollution also can irritate your lungs, so check daily air quality forecasts before going out. Identify what may trigger bouts of worsening symptoms so you can avoid them as much as possible.
- See your healthcare professional regularly. Keep your appointment schedule, even if you’re feeling fine. It’s important to regularly monitor your lung function. And be sure to get your annual flu vaccine in the fall to help prevent infections that can worsen your COPD. Ask your healthcare professional about when to get the pneumococcal vaccine, COVID-19 vaccine and RSV vaccine. Call your healthcare professional if your symptoms get worse or you notice symptoms of infection.
You might want to take a friend or family member with you to the appointment to help you remember information.
Before your appointment, make a list of:
- Symptoms you’re experiencing and when they started. Include anything that makes your symptoms worse or better.
- All medicines, vitamins, herbs and supplements you take. Include the doses.
- Family history, such as whether anyone in your family has COPD.
- Treatment you’ve had for COPD, if any. Include what the treatment was and if it helped.
- Any other medical conditions you have and their treatments.
- If you smoke or have ever smoked.
- Questions to ask your healthcare professional.
Questions to ask may include:
- What is likely causing my symptoms?
- What kinds of tests do I need?
- What treatment do you recommend?
- I have other health conditions. How will COPD affect them?
- Are there any restrictions that I need to follow?
Feel free to ask other questions during your appointment.
Your healthcare professional may ask you questions, such as:
- How long have you had a cough?
- Do you find it hard to catch your breath, even with little or no activity?
- Have you noticed any wheezing when you breathe?
- Do you now or have you ever smoked cigarettes? If you smoke, would you like help in quitting?

Related Topics
Good Habits You Should Know
Bad Habits You Should Know
References
- COPD. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health/copd. Accessed March 13, 2024.
- Nici L, et al. Pharmacologic management of chronic obstructive pulmonary disease: An official American Thoracic Society clinical practice guideline. American Journal of Respiratory and Critical Care Medicine. 2020; doi:10.1164/rccm.202003-0625ST.
- Ferri FF. Chronic obstructive pulmonary disease. In: Ferri’s Clinical Advisor 2024. Elsevier; 2024. https://www.clinicalkey.com. Accessed March 13, 2024.
- Park HM, et al. In vitro delivery efficiencies of nebulizers for different breathing patterns. BioMedical Engineering OnLine. 2021; doi:10.1186/s12938-021-00895-3.
- Goldman L, et al., eds. Chronic obstructive pulmonary disease. In: Goldman-Cecil Medicine. 27th ed. Elsevier; 2024. https://www.clinicalkey.com. Accessed March 13, 2024.
- Wingardh ASL, et al. Effectiveness of energy conservation techniques in patients with COPD. Respiration. 2020; doi:10.1159/000506816.
- Broaddus VC, et al., eds. COPD: Pathogenesis and natural history. In: Murray and Nadel’s Textbook of Respiratory Medicine. 7th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed March 13, 2024.
- Broaddus VC, et al., eds. COPD: Diagnosis and management. In: Murray and Nadel’s Textbook of Respiratory Medicine. 7th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed March 13, 2024.
- Janjua S, et al. Prophylactic antibiotics for adults with chronic obstructive pulmonary disease: A network meta-analysis. Cochrane Database of Systematic Reviews. 2021; doi:10.1002/14651858.CD013198.pub2.
- Agustí A, et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. American Journal of Respiratory and Critical Care Medicine. 2023; doi:10.1164/rccm.202301-0106PP.
- Nagata K, et al. Home high-flow nasal cannula oxygen therapy for stable hypercapnic COPD. American Journal of Respiratory and Critical Care Medicine. 2022; doi:10.1164/rccm.202201-0199OC.
- Allscripts EPSi. Mayo Clinic.
- Medical review (expert opinion). Mayo Clinic. June 5, 2024.
- Medical review (expert opinion). Mayo Clinic. July 17, 2024.
-
Find a clinic near you
-
Call for an appointment!
-
Feel free to message us!
About Us
Curafile is the biggest Healthcare Curated Network Globally that serves citizens, service providers in B2C and B2B directions.
- Al Hussain Business Park
Amman, Jordan
Additional Links
- test October 20, 2025
- Hello world! October 7, 2025
- Many doctors use wrong test to diagnose kids food allergies February 12, 2017
- Rising cost of diabetes care concerns patients and doctors January 15, 2017
- Can breakfast help keep us thin? Nutrition science is tricky January 5, 2017
