Protein in Urine
- Home
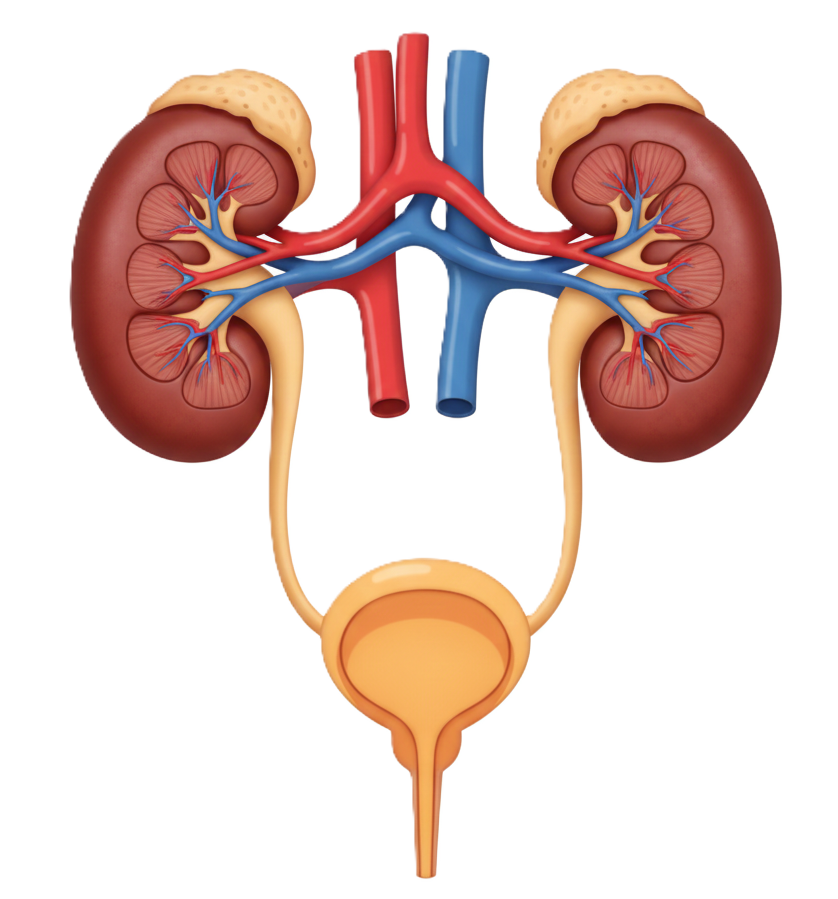
- Kidneys and Urinary System
- Protein in Urine
Protein in your urine (proteinuria) can be a sign that protein is getting past your kidneys’ filtration system and leaving your body in your pee. It can make your pee look foamy or bubbly. Kidney disease, diabetes, autoimmune disorders, preeclampsia and other serious conditions can cause it. Other causes include dehydration and fever.
-
What Is Protein in Your Urine
(Proteinuria)? -
What are the types of
proteinuria? -
What level of protein in your
urine is concerning?
Protein in your urine (proteinuria) happens when proteins like albumin, that are normally found in your blood, leak into your pee (urine). Your kidneys usually prevent this from happening.
But kidney disease or other chronic conditions can damage them, allowing proteins to leave your body through your pee. Other, less serious conditions can also sometimes cause temporary proteinuria.
Proteinuria is also called albuminuria.
There are three main types of proteinuria:
- Transient: This is intermittent (on and off) protein in your urine, or proteinuria that goes away on its own. Temporary conditions — like fever, stress or intense exercise — usually cause it.
- Orthostatic: Some people have higher levels of protein in their pee after they’ve been sitting or standing for a long time, but normal levels after they’ve been lying down. This can happen in younger people, especially if they’re tall and slim.
- Persistent: If you have multiple urine tests over time that show protein in your pee, you have persistent proteinuria. This can be a sign of a more serious condition, like kidney disease.
A normal amount of protein in your urine is less than 150 milligrams (mg) per day. Proteinuria is more than 150 mg of protein in your pee. Always check the reference range on your test results, as this number can vary depending on the lab.
If you have 3 to 3.5 grams (3,000 to 3,5000 mg) of protein in your pee per day, you have nephrotic-range proteinuria. Nephrotic syndrome is a relatively rare condition that causes your kidneys to release an excessive amount of protein in your pee.
You may notice foamy pee or bubbles in your pee if you have proteinuria. But small amounts of protein in your urine usually don’t cause symptoms.
If you’re losing a large amount of protein, your kidneys may be damaged. This can mean there’s too little protein in your blood. This can cause symptoms like:
- Swelling (edema) in your face, belly, feet or ankles
- Shortness of breath
- Tiredness
- Nausea and vomiting
- Lack of appetite
- Muscle cramping at night
- Puffiness around your eyes, especially in the morning
-
What does protein in
your urine mean? - What causes it?
High levels of protein in your pee can mean that your kidneys aren’t working properly — but it doesn’t always mean that. Protein travels through your body in your blood to perform a variety of functions. Your blood flows through tiny blood vessels in your kidneys (glomeruli), which filter out waste. The waste leaves your body in your pee.
Proteins shouldn’t be able to pass through your glomeruli (“gluh-MEHR-yuh-lie”) and enter your pee. But if they do slip through, long, thin tubes called tubules recover them and return them to your blood.
If you have a lot of protein in your urine, it means that your kidneys are allowing it to leak out of your blood. This could happen because of damage to your glomeruli or tubules. Sometimes, it means that there’s a problem with the way your body reabsorbs the proteins.
Causes of protein in your urine range from temporary conditions to serious and long-lasting diseases. Causes include:
- Dehydration
- Conditions that affect your kidneys, like kidney stones, inflammation (glomerulonephritis), infection, cancer and chronic kidney disease
- Diabetes-related kidney disease
- Certain autoimmune disorders, including lupus and rheumatoid arthritis
- Multiple myeloma, a type of blood cancer
- Destruction of red blood cells (hemolysis)
- Cardiovascular disease
- High blood pressure that’s not managed
- Preeclampsia, a serious condition that causes high blood pressure and organ damage during pregnancy or after birth
- Drug or toxin poisoning (like heavy metal poisoning)
- Congestive heart failure
Intense exercise, stress, taking aspirin and other anti-inflammatory medications (like ibuprofen) every day can cause protein to leak into your urine. Cold temperatures can also trigger proteinuria.
Your healthcare provider diagnoses proteinuria with a urine test. You’ll pee in a cup, and your provider tests it with a dipstick that changes color if protein is in your urine. This is usually part of a urinalysis, where a provider checks the appearance of your pee and looks for blood cells, bits of proteins (casts) and other substances.
Providers treat the cause of protein in your urine rather than proteinuria itself. Depending on the cause, your provider may recommend:
- Medication, including those that suppress your immune system or directly reduce protein in your urine
- Treatment for diabetes and high blood pressure
- Quitting smoking
- Changing the foods you eat
- Dialysis if your kidneys fail
- In severe cases, a kidney transplant
Some causes of protein in your urine don’t need treatment.
What are the possible complications of untreated proteinuria?
If you have a condition that’s causing kidney damage, your kidneys could fail if you’re not treated promptly. Chronic kidney disease can also lead to other complications, including:
- Heart and blood vessel disease
- High blood pressure
- High cholesterol levels
- Nerve damage
- Bone thinning (osteoporosis)
Contact your healthcare provider if you:
- Are peeing more often than you usually do
- Have pain when you pee
- Have foamy or bubbly pee
- Feel dizzy, weak or lightheaded
- Have shortness of breath
- Have swelling or puffiness around your face, belly or lower body
- Have symptoms that don’t improve after treatment
References
- American Kidney Fund. Protein in Urine (Proteinuria) Causes, Symptoms, & Treatments (https://www.kidneyfund.org/all-about-kidneys/other-kidney-problems/protein-urine).). Last updated 8/24/2024. Accessed 11/13/2025.
- Uehara K, Tominaga N, Shibagaki Y. Adult orthostatic proteinuria (https://pubmed.ncbi.nlm.nih.gov/25852903/). Clin Kidney J. 2014 Jun;7(3):327-8. Accessed 11/13/2025.
- Winter WE. The Kidney. In: Laposata M, ed. Laposata’s Laboratory Medicine: Diagnosis of Disease in the Clinical Laboratory. 3rd ed. McGraw-Hill Education; 2019.

Ad
Women have unique health issues. And some of the health issues that affect both men and women can affect women differently.
Check the latest Healthcare NEWS!
Nothing more important than keeping yourself updated with the latest in Health!
Go to NEWS-
Find a healthcare provider near you
-
Call for support
-
Feel free to message us!
About Us
Curafile is a Medical Cyclopedia, biggest Healthcare Curated Network Globally, serves citizens, service providers in one place.
- Estonia - Qatar
Jordan - Saudi Arabia