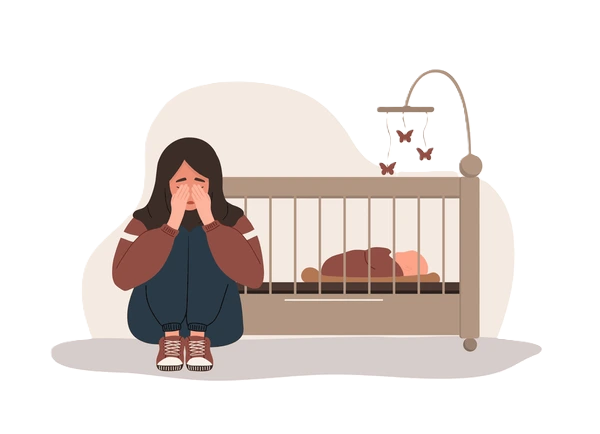
Postpartum depression is a type of depression that happens after having a baby. It affects up to 15% of women. Postpartum depression involves emotional highs and lows, frequent crying, fatigue, guilt and anxiety. You may have trouble caring for your baby. Postpartum depression can be treated with medication and counseling.
What is postpartum depression?
Having a baby is a life-changing experience. Being a parent is exciting but can also be tiring and overwhelming. It’s normal to have feelings of worry or doubt, especially if this is your first time. But if your feelings include extreme sadness or loneliness, severe mood swings and frequent crying spells, you may have postpartum depression.
Postpartum depression (PPD) is a type of depression that happens after you give birth. Postpartum depression doesn’t just affect the birth mother. It can affect surrogates and adoptive parents, too. It’s common to experience hormonal, physical, emotional, financial and social changes after having a baby. These changes can cause symptoms of postpartum depression.
If you have postpartum depression, know that you’re not alone. It’s not your fault. And that help is out there. Your healthcare provider can manage your symptoms and help you feel better.
What are the types of postpartum depression?
There are three different types of postpartum mood disorders:
Postpartum blues or baby blues
The baby blues affect between 50% and 75% of women after delivery. If you’re experiencing the baby blues, you will have frequent, prolonged bouts of crying for no apparent reason, sadness and anxiety. The condition usually begins in the first week (one to four days) after delivery. Although the experience is unpleasant, the condition usually subsides within two weeks without treatment. The best thing you can do is find support and ask for help from friends, family or your partner.
Postpartum depression
Postpartum depression is a far more serious condition than the baby blues, affecting about 1 in 7 new moms. If you’ve had postpartum depression before, your risk increases to 30% each pregnancy. You may experience alternating highs and lows, frequent crying, irritability and fatigue, as well as feelings of guilt, anxiety and inability to care for your baby or yourself. Symptoms range from mild to severe and may appear within a week of delivery or gradually, even up to a year later. Although symptoms can last several months, treatment with psychotherapy or antidepressants is very effective.
Postpartum psychosis
Postpartum psychosis is an extremely severe form of postpartum depression and requires emergency medical attention. This condition is relatively rare, affecting only 1 in 1,000 women after delivery. The symptoms generally occur quickly after delivery and are severe, lasting for a few weeks to several months. Symptoms include severe agitation, confusion, feelings of hopelessness and shame, insomnia, paranoia, delusions or hallucinations, hyperactivity, rapid speech or mania. Postpartum psychosis requires immediate medical attention since there is an increased risk of suicide and risk of harm to the baby. Treatment will usually include hospitalization, psychotherapy and medication.
Who is affected by postpartum depression?
Postpartum depression is common. As many as 75% of women experience baby blues after delivery. Up to 15% of these individuals will develop postpartum depression. One in 1,000 women develop postpartum psychosis.
How do I know if I have baby blues or postpartum depression?
It’s common to have baby blues after giving birth. Baby blues and postpartum depression have similar symptoms. However, symptoms of baby blues last about 10 days and are less intense. With postpartum depression, the symptoms last weeks or months, and the symptoms are more severe.
You may have the baby blues if you:
- Have crying spells
- Feel overwhelmed
- Lose your appetite
- Have trouble sleeping
- Have sudden mood changes
Remember, it doesn’t hurt to share your symptoms with your provider. They can assess if you need treatment for your symptoms.
How long does postpartum depression last?
Postpartum depression can last until one year after your child is born. However, this doesn’t mean you should feel “cured” in one year. Talk to your healthcare provider about your symptoms and treatment. Be honest about how you feel. Think carefully about if you feel better than you did at the beginning of your diagnosis. Then, they can recommend ongoing treatment for your symptoms.
What factors increase my risk of being depressed after the birth of my child?
Certain factors increase your risk for postpartum depression:
- Having a personal or family history of depression, postpartum depression or premenstrual dysphoric disorder (PMDD)
- Limited social support
- Marital or relationship conflict
- Ambivalence about the pregnancy
- Pregnancy complications like health conditions, difficult delivery or premature birth
- You’re younger than 20 or a single parent
- Having a baby with special needs or a baby who cries a lot
You might feel ashamed about your symptoms or feel you’re a terrible mom for feeling the way you do. Postpartum depression is extremely common. You’re not the only one who feels this way, and it doesn’t mean you’re a bad person.
You may have postpartum depression if you experience some of the following:
- Feeling sad, worthless, hopeless or guilty
- Worrying excessively or feeling on edge
- Loss of interest in hobbies or things you once enjoyed
- Changes in appetite or not eating
- Loss of energy and motivation
- Trouble sleeping or wanting to sleep all the time
- Crying for no reason or excessively
- Difficulty thinking or focusing
- Thoughts of suicide or wishing you were dead
- Lack of interest in your baby or feeling anxious around your baby
- Thoughts of hurting your baby or feeling like you don’t want your baby
Contact your healthcare provider if you think you have postpartum depression. This can be your obstetrician, primary care provider or mental health provider. Your baby’s pediatrician can also help you.
More research is needed to determine the link between the rapid drop in hormones after delivery and depression. The levels of estrogen and progesterone increase tenfold during pregnancy but drop sharply after delivery. By three days postpartum, levels of these hormones drop back to pre-pregnancy levels.
In addition to these chemical changes, the social and psychological changes associated with having a baby increase your risk of postpartum depression. Examples of these changes include physical changes to your body, lack of sleep, worries about parenting or changes to your relationships.
If you’ve had any of the following symptoms, please notify your healthcare provider right away:
- Thoughts of harming yourself or your baby
- Recurrent thoughts of death or suicide
- Depressed mood for most of the day, nearly every day for the last two weeks
- Feeling anxious, guilty, hopeless, scared, panicked or worthless
- Difficulty thinking, concentrating, making decisions or dealing with everyday situations
- Loss of interest or pleasure in most activities nearly every day for the last two weeks
Can postpartum depression affect my baby?
Yes, postpartum depression can affect your baby. Getting treatment is important for both you and your baby.
Research suggests that postpartum depression can affect your baby in the following ways:
- You have trouble bonding with your baby and don’t establish a connection with them.
- Your child may have behavior or learning problems.
- You may skip appointments with your child’s pediatrician.
- Your child may have feeding and sleeping issues.
- Your child may be at higher risk for obesity or developmental disorders.
- You may neglect your child’s care or not recognize when they are ill.
- Your baby may have impaired social skills.
There isn’t a specific test that diagnoses postpartum depression. Your healthcare provider will evaluate you at your postpartum visit. This visit may include discussing your health history, how you’ve felt since delivery, a physical exam, pelvic exam and lab tests. Many providers schedule visits at two or three weeks postpartum to screen for depression. This ensures you get the help you need as soon as possible.
They may do a depression screening or ask you a series of questions to assess if you have postpartum depression. They’ll ask how you’re feeling and how your baby is doing. Be open and honest with your provider to ensure they get an accurate picture of your emotions and thoughts. They can help distinguish if your feelings are typical or symptoms of postpartum depression.
Your healthcare provider may order a blood test because postpartum depression can cause symptoms similar to many thyroid conditions.
Remember, your healthcare provider is there to support you and make sure you are healthy, so be honest with them. There is no judgment, and you aren’t alone in your feelings.
How do doctors screen for postpartum depression?
It can be hard to detect mild cases of postpartum depression. Healthcare providers rely heavily on your responses to their questions.
Many healthcare providers use the Edinburgh Postnatal Depression Scale to screen for postpartum depression. It consists of 10 questions related to symptoms of depression such as feeling unhappy, anxious or guilty. You’re asked to check the response that comes closest to how you’ve felt the last seven days. A higher score indicates possible postpartum depression.
If your provider feels you have signs of postpartum depression, they will recommend an appropriate treatment.
Postpartum depression is treated differently depending on the type and severity of your symptoms. Treatment options include anti-anxiety or antidepressant medicines, psychotherapy (talk therapy or cognitive behavioral therapy) and support group participation.
Treatment for postpartum psychosis may include medication to treat depression, anxiety and psychosis. You may also be admitted to a treatment center for several days until you’re stable. If you don’t respond to this treatment, electroconvulsive therapy (ECT) can be effective.
If you are breastfeeding, don’t assume that you can’t take medicine for depression, anxiety or even psychosis. Talk to your healthcare provider about your options.
What medications can I take for postpartum depression?
Your healthcare provider may prescribe antidepressants to manage symptoms of postpartum depression. Antidepressants help balance the chemicals in your brain that affect your mood.
If you’re breastfeeding, talk to your healthcare provider about the risks and benefits of taking an antidepressant. Medications can transfer to your baby through your milk. However, the transfer level is generally low, and many antidepressant medications are considered safe. Your provider can help you decide what medicine is right for you based on your symptoms and if you’re nursing.
Some common antidepressants for postpartum depression are:
- Selective serotonin reuptake inhibitors, like sertraline and fluoxetine
- Serotonin and norepinephrine reuptake inhibitors (SNRIs), like duloxetine and desvenlafaxine
- Bupropion
- Tricyclic antidepressants (TCAs), like such as amitriptyline or imipramine
Keep in mind that it takes at least three or four weeks for antidepressants to work. Talk to your healthcare provider before stopping the medication. Stopping your medication too soon can cause symptoms to return. Most providers will recommend reducing your dose before stopping completely.
If your provider detects postpartum depression while you’re still in the hospital, they may recommend IV medication containing brexanolone.
What are ways to cope with postpartum depression?
It’s OK to feel overwhelmed. Parenting is full of ups and downs and having a baby isn’t easy. If you have depression, you’re not alone. Your healthcare provider can help find a treatment that works for you.
Here are some things you can do to help cope with postpartum depression:
- Find someone to talk to — a therapist, friend, family member or someone who will listen to you and help you
- Join a support group for new parents
- Try to eat healthily and find time for exercise
- Prioritize rest for yourself
- Go out with friends or talk to them on the phone
- Find time for self-care and doing things you enjoy, like reading or other hobbies
- Get help with household chores or errands
What happens if postpartum depression isn’t treated?
Untreated postpartum depression is dangerous and affects you, your baby and those who love you. It can make you:
- Feel like you have no energy
- Moody
- Believe you can’t take care of your baby
- Unable to focus or make decisions
- Have thoughts of hurting yourself
With professional help, almost all those who experience postpartum depression can overcome their symptoms.
Postpartum depression isn’t entirely preventable. It helps to know warning signs of the condition and what factors increase your risk. Here are some tips that can help prevent postpartum depression:
- Be realistic about your expectations for yourself and your baby
- Limit visitors when you first go home
- Ask for help — let others know how they can help you
- Sleep or rest when your baby sleeps
- Exercise — take a walk and get out of the house for a break
- Keep in touch with your family and friends — don’t isolate yourself
- Foster your relationship with your partner — make time for each other
- Expect some good days and some bad days
References
- ACOG. Postpartum depression (https://www.acog.org/womens-health/faqs/postpartum-depression). Accessed 4/13/2022.
- American Academy of Family Physicians. Postpartum Depression (PPD) (https://familydoctor.org/condition/postpartum-depression/). Accessed 4/13/2022.
- American Psychiatric Association. What is Postpartum Depression? (https://www.psychiatry.org/patients-families/postpartum-depression/what-is-postpartum-depression) Accessed 4/13/2022.
- American Psychological Association. What is Postpartum Depression and Anxiety? (https://www.apa.org/pi/women/resources/reports/postpartum-depression) Accessed 4/13/2022.
- Centers for Disease Control. Depression During and After Pregnancy (https://www.cdc.gov/reproductivehealth/features/maternal-depression/index.html). Accessed 4/13/2022.
- Complojer M, Schweigkofler H, Schwitzer J, Scherer A, Schwitzer GO, Schiefenhövel W. Die Bedingungsvariablen der postpartalen Dysphorie [The preconditions of postpartum dysphoria (https://pubmed.ncbi.nlm.nih.gov/19272290/)]. Neuropsychiatr. 2009;23(1):35-41. German. PMID: 19272290. Accessed 4/13/2022.
- March of Dimes Foundation. Postpartum depression (https://www.marchofdimes.org/pregnancy/postpartum-depression.aspx). Accessed 4/13/2022.
- National Institute of Mental Health. Perinatal depression. (https://www.nimh.nih.gov/health/publications/perinatal-depression) Accessed 4/13/2022.
- Office on Women’s Health. Postpartum depression (https://www.womenshealth.gov/mental-health/mental-health-conditions/postpartum-depression). Accessed 4/13/2022.
- U.S. Preventative Services Tash Force. Recommendation: Perinatal Depression Prevention Interventions (https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/perinatal-depression-preventive-interventions#fullrecommendationstart). Accessed 4/13/2022.
Related Topics

Other Specialities
Stay away from bad habbits
Mental Health
Mental health includes our emotional, psychological, and social well-being. It affects how we think, feel, and act as we cope with life.
Book your appointment TODAY!
Search on the closest Doctor to your location and book based on specialty. EARN 10 POINTS more with CuraPOINT.
BOOK-
Find a healthcare provider near you
-
Call for support
-
Feel free to message us!
About Us
Curafile is the biggest Healthcare Curated Network Globally that serves citizens, service providers in one place.
- Estonia - Qatar
Jordan - Saudi Arabia