Cornea Transplant
- Home
- Transplantation and Donation
- Cornea Transplant
Cornea transplant, also called corneal grafting, replaces a damaged cornea with tissue from a deceased donor. A cornea transplant can treat conditions such as Fuchs’ dystrophy and keratoconus. Most people have improved vision and less pain.
- What is a cornea transplant?
-
What conditions can you treat
with a cornea transplant? - How common are corneal transplants?
Cornea transplant (corneal transplant) is surgery to replace your cornea, the clear front layer of your eye. Corneal grafting and keratoplasty are other terms for cornea transplant.
Your eye care provider may recommend you consider a cornea transplant if you’ve damaged your cornea. Cornea damage causes eye pain, cloudy and blurred vision.
In a cornea transplant, your surgeon removes your damaged cornea and replaces it with donated healthy corneal tissue. For many people, cornea transplant surgery restores vision and improves their quality of life.
Your eye care provider may suggest a cornea transplant if you have:
- Fuchs’ dystrophy.
- Keratoconus.
- Corneal ulcers or other damage to the cornea from injuries, inflammation and infections.
- Corneal damage caused by earlier eye surgery.
- Bullous keratopathy, a blister-like swelling of the cornea.
There are about 185,000 cornea transplant surgeries performed every year throughout the world. In the U.S., ophthalmologists perform more than 47,000 corneal transplants annually. The top three countries for these procedures are:
- The United States.
- Lebanon.
- Canada.
People living in more than half of the countries in the world don’t have access to this surgery. One reason for this is the lack of donated corneas. There’s only one cornea available for every 70 individuals in need.
There are three surgical options for cornea transplant: penetrating keratoplasty, deep anterior lamellar keratoplasty and endothelial keratoplasty. Your cornea has three layers of tissue. Each of these surgeries targets a specific layer or layers of tissue.
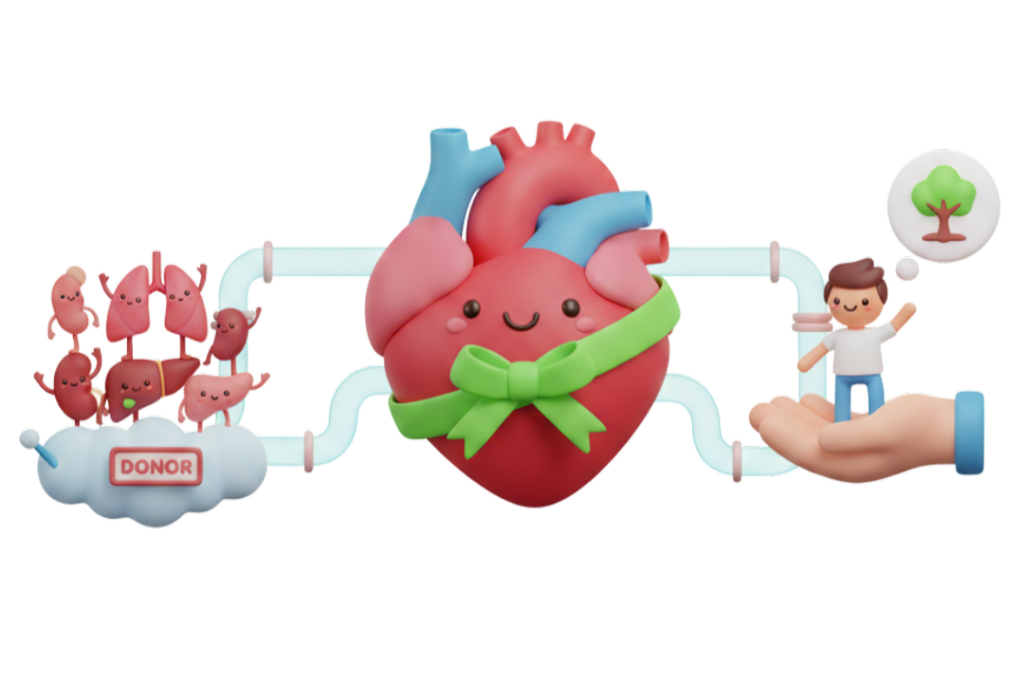
All corneal transplants use corneas from deceased human organ donors. Every donor cornea undergoes thorough testing to make sure it’s safe for transplant.
- Penetrating keratoplasty
- Deep anterior lamellar keratoplasty
- Endothelial keratoplasty
Another term for penetrating keratoplasty is full-thickness cornea transplantation. Developed over 100 years ago, the modern version of this surgery continues to help thousands of people each year. In this procedure, your surgeon uses a small circular blade to remove the entire center part of the damaged cornea and replaces it with a healthy, same-shaped piece of donor cornea.
If the innermost layer of your cornea is healthy and the damage lies in the middle and outer layers, your surgeon may perform a partial thickness cornea transplant. Another term for this is a deep anterior lamellar keratoplasty. During this surgery, your surgeon removes the middle and outer layers of your cornea and replaces them with healthy donated corneal tissue.
This surgery may help if you have damage on the innermost layer of your cornea, the endothelium, which rests on Descemet’s membrane. Surgeons perform two types of endothelial keratoplasty surgeries:
- Descemet’s stripping automated endothelial keratoplasty (DSAEK).
- Descemet’s membrane endothelial keratoplasty (DMEK).
Both surgeries involve removing damaged endothelial tissue and replacing it with healthy donor tissue. The difference between DSAEK and DMEK is the thickness of the donor cornea — DSAEK is thicker, while DMEK is thinner. You and your surgeon will decide which type of transplant is best for your specific eye condition.
Endothelial keratoplasty procedures require fewer sutures than other keratoplasty procedures. Instead, the technique uses an air bubble to keep the donor cornea in position. To increase the chance of success, you’ll need to make sure you’re lying face up when you rest or sleep for the first few days after surgery. Lying face up helps the air bubble keep your transplanted corneal tissue in place.
-
How should I prepare for
a cornea transplant? -
What happens during
a cornea transplant? -
What happens after
a cornea transplant?
Your surgeon and the anesthesia team will review your medical history, answer your questions and confirm the surgical plan. They’ll let you know if you need to stop taking any medications or over-the-counter (OTC) products before your surgery. They’ll also tell you when to stop eating and drinking before the surgery. You’ll need transportation home after surgery since you won’t be able to drive.
The anesthesia team will administer either sedation or general anesthesia (making you unconscious), depending on your medical condition and what you and your healthcare provider have discussed. A caregiver will apply numbing medication to your eye.
You’ll need a driver to take you home after you leave the recovery unit. You may want someone to spend the evening with you. You’ll need to wear an eye patch when you leave.
- For the first few days after surgery, your eye will be red, irritated and sensitive to light. You can manage your pain with over-the-counter pain relief products that your surgeon recommends.
- You must wear your eye patch after your surgery as directed by your surgeon.
- If you have an endothelial transplant, you’ll have to stay in position with your face up (on your back) for a few days after surgery.
- Your surgeon will let you know about activities that you should avoid, especially activities that increase your risk that something will hit your eye.
- You’ll have a follow-up visit with your surgeon, usually within 24 to 48 hours of your surgery. They’ll remove your eye patch and check on how well your eye is healing.
- You’ll get prescription eye drops and, in some cases, ointments to help your eye heal. These medications are usually antibiotics (to prevent infection) and corticosteroids (to reduce swelling, inflammation and to prevent rejection).
- Depending on the type of stitches and the operation you’ve had, you may or may not have to have stitches removed. Some stitches may stay in for several months.
- Your surgeon will recommend that you wear glasses or other protective eyewear for some time to help protect your eyes. While you recover, don’t rub or press on your eyes. Rubbing can cause damage and interfere with healing.
- After surgery, you should contact your eye care provider if you have problems.
Complications associated with a lung transplant can be serious and sometimes fatal. Major risks include rejection and infection.
-
What are the benefits of
a cornea transplant? -
What are cornea transplant
complications?
Most people who have a cornea transplant see more clearly. In rare circumstances, you may have a cornea transplant to reduce eye pain.
A cornea transplant is generally a very safe surgery. Your surgical team will make every effort to reduce your risk of complications.
One of the most concerning complications of cornea transplant is organ (cornea) rejection. Rejection means your body’s immune system identifies the donated cornea as foreign and tries to fight off the transplant. Risk of rejection varies based on the surgical technique used and on the condition of your eye.
In some cases, your surgeon may recommend against surgery because your eye is likely to reject a transplanted cornea. Conditions like severe dry eye, blood vessels growing in the cornea and eye infections increase the chance of rejection.
If you have a cornea transplant, you’ll need to use eye drops for at least a year following surgery to reduce the risk of rejection.
Other complications of cornea transplant surgery include:
- Infection in the cornea or inside the eye.
- Bleeding.
- Glaucoma (increased pressure inside your eye).
- Fluid leakage from your cornea.
- Detached retina.
- Visual acuity (sharpness of your vision) problems due to an irregular curve in the shape of the cornea.
- Detachment of the cornea transplant (for an endothelial transplant, which is held in place by an air bubble).
-
What is the outlook (prognosis)
for people who have a cornea transplant? - How soon can I drive after a cornea transplant?
- When can I return to work after a cornea transplant?
The degree of long-term success depends on a number of factors, including:
- The underlying cause of the cornea damage.
- The surgical technique used.
- Expertise of your surgical team.
- Your immune system acceptance of the donor transplant (organ rejection).
Because success varies, you should ask your surgeon what you might expect given your particular situation, including your eye health.
Keep in mind that you’ll probably have blurred vision after surgery that will gradually improve over time. Several factors affect how long it’ll take for the vision in your eye to return to normal.
For example, if you had a full-thickness transplant, it may take up to 12 months for you to have full vision. But if you had an endothelial transplant (DMEK or DSAEK), you may achieve good vision within three months.
You can’t drive on the day of your cornea transplant. Someone needs to drive you home after surgery and bring you back for your follow-up visit.
If you have good vision in the non-transplant eye, you can legally drive 24 hours after surgery. However, your surgeon may recommend waiting longer before driving, especially if you had an endothelial transplant.
It may take a few days to a few weeks before you can return to work. It depends on your level of discomfort, your vision and what activities you perform at work. If your job involves strenuous activities like lifting heavy objects, you may need to take additional time away from work.
Contact your surgeon immediately if you experience any signs of cornea rejection, including:
- Eye pain.
- Eye redness.
- Hazy or cloudy vision.
- Sensitivity to light.
Contact your surgeon if you notice any other problems in your vision after cornea transplant, or you experience symptoms of infection, such
References
- American Academy of Ophthalmology. About Corneal Transplantation (https://www.aao.org/eye-health/treatments/about-corneal-transplantation). Accessed 3/9/2023.
- Centers for Disease Control and Prevention. Tips to Prevent Vision Loss (https://www.cdc.gov/visionhealth/risk/tips.htm). Accessed 3/9/2023.
- Cornea Research Foundation of America. Endothelial Keratoplasty (DSEK & DMEK) (http://www.cornea.org/Learning-Center/Cornea-Transplants/Endothelial-Keratoplasty.aspx). Accessed 3/9/2023.
- Merck Manual Professional Version. Corneal Transplantation (http://www.merckmanuals.com/professional/eye-disorders/corneal-disorders/corneal-transplantation). Accessed 3/9/2023.
- National Eye Institute. Corneal (https://nei.nih.gov/health/cornealdisease/) Conditions. Accessed 3/9/2023.
- Saving Sight. Important Information about Cornea Donation (https://saving-sight.org/cornea-donation-facts). Accessed 3/9/2023.

Ad
Women have unique health issues. And some of the health issues that affect both men and women can affect women differently.
Book your appointment TODAY!
Search on the closest Doctor to your location and book based on specialty. EARN 10 POINTS more with CuraPOINT.
BOOK-
Find a healthcare provider near you
-
Call for support
-
Feel free to message us!
About Us
Curafile is the biggest Healthcare Curated Network Globally that serves citizens, service providers in one place.
- Estonia - Qatar
Jordan - Saudi Arabia